- 如有疑问,请联系电邮
- customer@ihealth66.com
USNEWS:对肺癌活检的重要性需要了解更多

USNEWS:需要了解年轻患者的肺癌原因
2019年3月28日
最新临床试验:联合化疗、贝伐单抗和/或阿替唑单抗治疗DNA错配修复转移性结直肠癌
2019年4月1日By Kathleen Hall
你的医生在影像学检查后发现你的肺部有可疑的东西。接下来会发生什么?如果有一个合理的怀疑,异常是癌症,你的医生会想做一个活组织检查来了解更多。
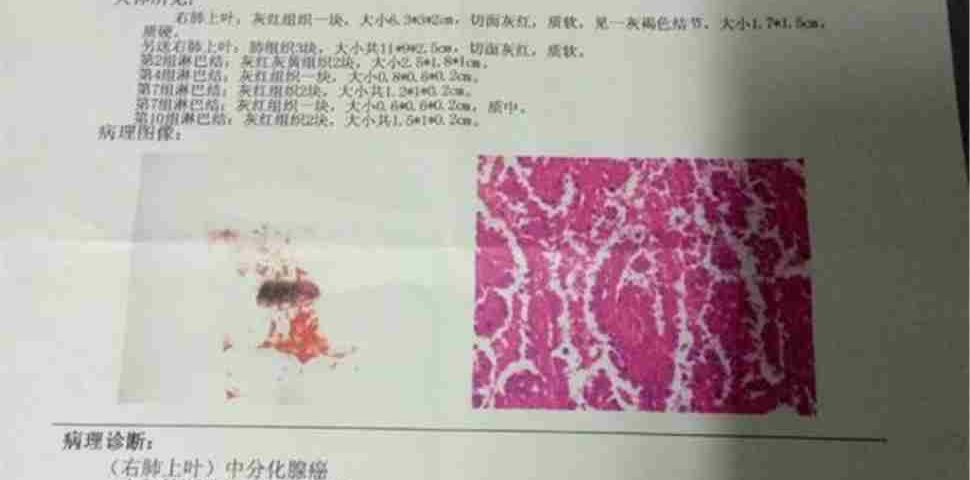
活检是在显微镜下取出一小块组织(有时是液体)进行检查的过程。组织样本可以帮助医生确认你患了癌症,并确定癌症的发展阶段。越来越多的病理学家也会对活检样本进行额外的药物敏感测试,看看你是否适合接受一些新的靶向肺癌治疗。
如何进行活检?
有几种方法可以确保组织样本的安全,但首先它有助于了解肺的布局。当你呼吸时,空气从你的鼻子或嘴巴进入你的气管(呼吸管)。气管分支到左右支气管,左右支气管进入肺部。支气管进一步分成越来越小的气道,当你进入肺的深处,离开气管。
医生说,决定活检程序的类型取决于肿块的位置。西奈山卫生系统(Mount Sinai Health System)的副教授卡迪纳莱·史密斯(Cardinale Smith)专门研究血液学和肿瘤学等领域。你的医生必须决定用什么技术来获得组织样本,然后如何收集它。
通常,医生使用支气管镜获取肺部组织样本。德克萨斯大学西南医学中心的肿瘤学家大卫·格伯说。支气管镜是一种薄管,有光和透镜,医生可以直接看到你的呼吸道。在支气管镜检查中,医生通过口腔或鼻子将一根管子插入喉咙。管子穿过气管和支气管进入肺部。
“当可疑的发现位于胸部中心时,我们会想到基于支气管镜的活检,”格伯说。如果肿块较周围(离气管或胸腔中心较远),支气管镜可能无法工作。
支气管镜检查允许医生通过以下两种方法之一获得组织样本:通过支气管镜插入小仪器(如针)从肿块中取出组织样本,或使用超声引导针。这叫做支气管内超声,简称EBUS。
Gerber说,EBUS是支气管镜的最新版本。“使用超声探头,你可以看到气管导管外的结构,而这些结构在其他情况下是看不见的(仅用支气管镜)。你可以寻找淋巴结,然后用针穿过(气道的)管壁进入淋巴结。”
另一种选择是经皮穿刺活检。在这个过程中,你将在一个扫描仪中,这样你的放射科医生可以实时看到针头的走向,戈贝尔说。这种类型的活检并不局限于肺部。它还被用于肝脏、肾上腺和骨骼的活组织切片检查,这些都是肺癌扩散的常见部位。
格伯说:“如果我们认为病人因为肝脏有肿块而患有4期肺癌(最严重的一种),我们可能会在那里做活检,而不是肺。”“这证明了(肺癌的)诊断和肺癌的分期。”
活检取样所用针的类型也很重要。当空间小的时候,小针是合适的。这叫做细针抽吸。核心活检使用更大的针来移除更大的组织样本。“你不会想让一根大针扎进肺里,”史密斯说。
有些病人可能会通过胸部前方的切口进行手术活检。“很少有病人接受这种手术,”史密斯说。“这取决于淋巴结的位置,例如,如果它们太远,无法用显微镜探测到。”
当然,进行侵入性手术总是有风险的,肺活检也不例外。用于提取组织样本的针越小,风险就越小。格伯说,位置和肺部健康也很重要。如果肿块一直在肺的边缘,你不需要穿过主肺才能得到样本,所以风险更小。如果你是一个烟瘾大的人或者有其他肺部疾病,并且你的肺部健康受到损害,那么并发症的风险就会更高。
新的靶向肺癌治疗方法既带来了机遇,也带来了挑战。新的治疗方法正在延长肺癌患者的寿命,有时效果显著,而此前肺癌患者的选择很少。然而,为了了解患者是否有可能对这些靶向治疗产生反应的特殊突变,病理学家必须对活检组织进行额外的检测,这意味着病理学家需要越来越大的组织样本。
YOUR DOCTOR HAS FOUND something suspicious in your lungs following an imaging test. What comes next? If there’s a reasonable suspicion the abnormality is cancer, your doctor will want to do a biopsy to learn more about it.
A biopsy is a procedure to remove a small bit of tissue (or, in some cases, fluid) to examine under a microscope. The tissue sample helps your doctor confirm you have cancer and determine what stage (how advanced) it is. Increasingly, pathologists also conduct additional tests on the biopsy sample to see if you’re a good candidate for some of the newer targeted lung cancer therapies.
How Is a Biopsy Performed?
There are several ways of securing a tissue sample, but first it helps to understand the layout of the lungs. When you breathe, the air travels from your nose or mouth down your trachea (breathing tube). The trachea branches into the left and right bronchi, which go into the lungs. The bronchi further divide into smaller and smaller airways as you go deeper into the lungs and away from the trachea.
The decision about the type of biopsy procedure depends on where the mass is, says Dr. Cardinale Smith, an associate professor at Mount Sinai Health System who specializes in hematology and medical oncology, among other topics. Your doctor must decide what technique to use to obtain the tissue sample and then how to collect it.
Usually, doctors use bronchoscopy to obtain a tissue sample in the lungs, says Dr. David Gerber, an oncologist at UT Southwestern Medical Center. A bronchoscopy is a thin tube with a light and a lens that allows your doctor to see directly into your airways. During a bronchoscopy, your physician inserts a tube down your throat through the mouth or nose. The tube passes through the trachea and the bronchi into the lungs.
“We think about bronchoscopic-based biopsy when the suspicious finding is central in the chest,” Gerber says. If the mass is more peripheral (farther away from the trachea or the center of the chest), a bronchoscope may not work.
A bronchoscopy allows the doctor to obtain a tissue sample in one of two ways: by inserting a small instrument, such as a needle, through the bronchoscope to remove a tissue sample from the mass, or by using an ultrasound to guide the needle. This is called endobronchial ultrasound, or EBUS.
EBUS is the newest edition of bronchoscopy, Gerber says. “With the ultrasound probe, you can see structures outside of the tubes of the airway that are otherwise invisible [with just the bronchoscopy]. You can look for lymph nodes and physically guide the needle through the wall [of the airway] into the lymph node.”
Another option is to perform a percutaneous (which means through the skin) needle biopsy. In this procedure, you will be in a scanner so your radiologist can visualize in real time where the needle is going, Gerber says. This type of biopsy is not limited to the lungs. It’s also used for biopsying the liver, adrenal gland and bone, which are common sites where lung cancer spreads.
“If we believe the patient has stage 4 lung cancer [the most advanced type] because there is a mass in the liver, we may do a biopsy there instead of the lung,” Gerber says. “This proves the diagnosis [of lung cancer] and the stage of the lung cancer.”
The type of needle used in biopsy sampling is important, too. A tiny needle is appropriate when the space is small. This is called fine needle aspiration. A core biopsy uses a bigger needle to remove a larger sample of tissue. “You don’t want a big needle in the lung,” Smith says.
Some patients may undergo surgical biopsy through an incision in the front of the chest. “Few patients get this procedure,” Smith says. “It depends on the location of the lymph nodes, for example, if they are too far to reach with a scope.”
Of course, there are always risks when you perform an invasive procedure, and lung biopsies are no exception. The smaller the needle used to withdraw the tissue sample, the less risky it is. Location and health of the lungs are important, too, Gerber says. If the mass is all the way on the edge of the lung, you don’t have to go through the main lung to get a sample, so it’s less risky. There’s a higher risk of complications if you were a heavy smoker or have other lung diseases and your lung health is compromised.
New targeted lung cancer therapies have created both an opportunity and a challenge. The new treatments are extending the life – sometimes significantly – of lung cancer patients who previously had few options. However, in order to know if a patient has special mutations that might respond to these targeted therapies, pathologists must do additional testing on biopsy tissue, which means pathologists need larger and larger tissue samples.