- 如有疑问,请联系电邮
- customer@ihealth66.com
USNEWS:糖尿病失控和胰腺癌之间有联系吗?

最新临床试验:伊布替尼和双珠单抗联合或不联合维奈托克治疗老年慢性淋巴细胞白血病
2019年3月18日
USNEWS:7种预防皮肤癌的方法
2019年3月20日By Vanessa Caceres
关于胰腺癌的事实可能是不明朗的。根据休斯顿德州大学安德森癌症中心癌症医学部胃肠内科肿瘤学教授Gauri Rajani Varadhachary博士的研究,胰腺癌占所有癌症病例的3%,但占所有癌症相关死亡的7%。
据美国癌症协会(American Cancer Society)的数据,在预计今年将被诊断为胰腺癌的美国53670人中,将有43000多人死于胰腺癌。
胰腺癌最近成为癌症死亡的第三大原因。到2020年,它有望成为第二大癌症死亡原因。
它之所以如此致命,是因为它在出现明显症状之前很难被发现。“它几乎总是在第4阶段被诊断出来。在那之前没有任何症状,”纽约威尔康奈尔医学院的肿瘤医生AllysonOcean博士说。第四阶段表明癌症是最高级的形式,到那时它已经扩散到身体的其他部位。
当你患有糖尿病时,你的健康状况比没有糖尿病的人更危险。这些包括高血压、视力下降和某些类型的癌症。但是,如果你突然出现不受控制的糖尿病,这是否意味着你患胰腺癌的风险更高?
底线:风险可能会更高一点,但这不是一个简单的答案。
首先,考虑数学。根据美国糖尿病协会的数据,每年有140万新的糖尿病诊断。然而,只有大约53000名新的胰腺癌患者。匹兹堡大学医学院副教授、匹兹堡希尔曼癌症中心的肿瘤学家和血液学家Nathan Bahary博士说,这意味着只有少数糖尿病患者会患胰腺癌。
如果你最近患了糖尿病,而且很难控制(这可能表明胰腺癌),医生会研究你可能有的其他危险因素,如胰腺癌家族史、胰腺炎、老年人、吸烟史和BRCA基因的存在。
根据胰腺癌行动网络的数据,糖尿病也是胰腺癌的一个危险因素,特别是那些已经患糖尿病5年以上的人。然而,不清楚为什么风险更高。“有两种理论,”巴尔的摩Medstar Franklin Square医疗中心的肿瘤学家Pallavi Kumar博士说。一种是胰腺癌引起糖尿病,另一种是与糖尿病有关的疾病促进癌症。
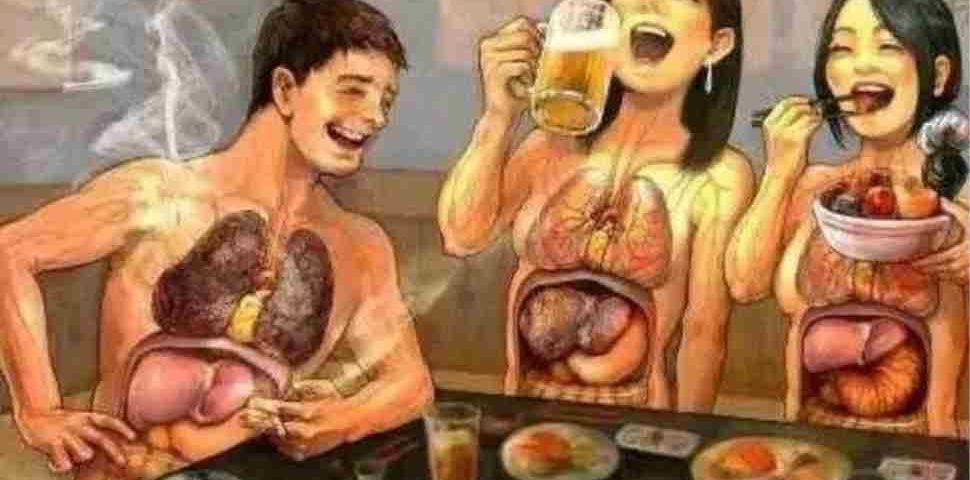
例如,许多胰腺癌和糖尿病患者的饮食和久坐的生活方式可能不好,这两种生活方式都会增加患癌症和糖尿病的风险,瓦拉达查里说。
Ocean说,医生还检查胰腺癌相关的症状,比如最近的体重减轻、腹部或背部疼痛和黄疸(皮肤变黄)。其他症状包括食欲下降、瘙痒和尿颜色变深。如果你有2型糖尿病症状和可能的胰腺癌,医生可能会考虑你如何不符合典型的2型糖尿病特征-例如,你是瘦的还是超重的,或者你比典型的2型糖尿病患者年轻。
库马尔说,控制不良的糖尿病的迅速发展也可能表明一些其他健康状况,如感染、肾脏问题、肝硬化和其他癌症。
如果你有控制不良的糖尿病和以上任何病史或症状,首先去看你的初级保健医生。巴哈里说:“他们是安检人员。”您的医生可能会要求进行基本的实验室工作,以跟踪您的完整血液计数、电解质和肝或肾功能。库马尔说:“如果病史、体检和血液检查都不正常,那么考虑成像就有必要了。”
医生会用CT扫描检查胰腺癌,有时还会做核磁共振检查。尽管并非所有确诊为糖尿病的新患者都建议对胰腺癌进行筛查,但Ocean相信,对于高危患者,如有胰腺癌家族史或有长期吸烟史的患者,筛查将变得更加普遍。
THE FACTS ABOUT pancreatic cancer can be bleak. Pancreatic cancer accounts for 3 percent of all cancer cases but 7 percent of all cancer-related deaths, according to Dr. Gauri Rajani Varadhachary, a professor at the Department of Gastrointestinal Medical Oncology, Division of Cancer Medicine at The University of Texas MD Anderson Cancer Center in Houston.
Of the predicted 53,670 people in the U.S. who will be diagnosed with pancreatic cancer this year, more than 43,000 will die from it, according to the American Cancer Society.
And pancreatic cancer recently became the third-leading cause of cancer deaths. By the year 2020, it’s expected to become the second-leading cause of cancer deaths.
The reason it’s so fatal is that it can be hard to detect until there are obvious symptoms. “It’s almost always diagnosed in stage 4. There are no symptoms until then,” says Dr. Allyson Ocean, a medical oncologist at Weill Cornell Medicine in New York. Stage 4 indicates a cancer’s most advanced form, and at that point it has spread to other parts of the body.
When you have diabetes, you’re at a higher risk for a number of health conditions than someone who doesn’t have the disease. These include high blood pressure, vision loss and certain types of cancer. But if you have a sudden onset of uncontrolled diabetes, does that mean you’re at a higher risk for pancreatic cancer?
The bottom line: The risk may be a little higher, but it’s not a simple answer.
First, consider the math. There are 1.4 million new diagnoses of diabetes each year, according to the American Diabetes Association. However, there are only about 53,000 new pancreatic cancer patients. That means only a small number of people with diabetes will have pancreatic cancer, says Dr. Nathan Bahary, an associate professor at the University of Pittsburgh School of Medicine and a medical oncologist and hematologist at Hillman Cancer Center in Pittsburgh.
If you recently developed diabetes, and it’s hard to control – which could indicate pancreatic cancer – doctors will look at other risk factors you may have, such as a family history of pancreatic cancer, pancreatitis, an older age, a history of smoking and presence of the BRCA gene.
Diabetes is also a risk factor for pancreatic cancer, especially in those who have had it for more than five years, according to the Pancreatic Cancer Action Network. However, it’s not clear why the risk is higher. “There are two theories,” says Dr. Pallavi Kumar, an oncologist with MedStar Franklin Square Medical Center in Baltimore. “One is that pancreatic cancer causes diabetes, and the second is that the conditions associated with diabetes promote cancer.”
For example, many patients with pancreatic cancer and diabetes may have a poor diet and a sedentary lifestyle, both of which can raise your cancer – and diabetes – risk, Varadhachary says.
Doctors also check for pancreatic cancer-associated symptoms, like recent weight loss, abdominal or back pain and jaundice (a yellowing of the skin), Ocean says. Other symptoms include decreased appetite, itching and darker urine. If you have symptoms of Type 2 diabetes and possible pancreatic cancer, doctors may consider how you don’t match the typical Type 2 diabetes profile – for example, you’re thin versus overweight or you’re younger than the typical person with Type 2 diabetes.
A rapid development of poorly controlled diabetes could also indicate a number of other health conditions, such as infection, kidney problems, liver cirrhosis and other cancers, Kumar says.
If you have poorly controlled diabetes and any of the history or symptoms above, start with a visit to your primary care doctor. “They’re the gate screeners,” Bahary says. Your doctor may order basic lab work that tracks your complete blood count, electrolytes and liver or kidney function. “If the history and physical and blood tests are abnormal, then a consideration of imaging may be warranted,” Kumar says.
Doctors will check for pancreatic cancer with a CT scan and sometimes an MRI. Although screening for pancreatic cancer is not recommended for all new patients diagnosed with diabetes, Ocean believes it will become more common in the future for higher-risk patients, such as those with a family history of pancreatic cancer or a long history of smoking.
At this point, the only way to treat pancreatic cancer is with surgery. However, doctors must first make sure surgery is the right choice for a specific patient. Pancreatic cancer surgery can have certain side effects, such as exocrine pancreatic insufficiency and diabetes.
Researchers are currently considering ways to screen for pancreatic cancer to catch it earlier with the use of blood biomarkers. A large trial supported by the National Institutes of Health, National Cancer Institute and National Institute for Diabetes and Digestive and Kidney Diseases is focused on better predicting the connection between pancreatitis, diabetes and pancreatic cancer. Different treatments for pancreatic cancer are also under investigation.
“Research progress has been slower than we want it to be,” Varadhachary says. However, oncologists are encouraged that there has been a great focus recently on pancreatic cancer research.
Ocean encourages those with pancreatic cancer to participate in clinical trials, which can help shed light on the best screenings and future treatments. Ask your doctor about available clinical trials or check out the clinical trials information on the Pancreatic Cancer Action network website.
To help lower your risk for cancer overall, try to eat healthy, lose weight if necessary and keep up with any regular cancer screenings recommended by your doctor. “We have to try to empower people before they get cancer. So much has to go into prevention,” Ocean says.
Best Hospitals for Diabetes & Endocrinology
|
RANK |
HOSPITAL NAME |
LOCATION |
|---|---|---|
|
#1
|
Mayo Clinic
|
Rochester, MN
|
|
#2
|
Massachusetts General Hospital
|
Boston, MA
|
|
#3
|
Cleveland Clinic
|
Cleveland, OH
|
|
#4
|
Johns Hopkins Hospital
|
Baltimore, MD
|
|
#5
|
New York-Presbyterian University Hospital of Columbia and Cornell
|
New York, NY
|
|
#6
|
UCSF Medical Center
|
San Francisco, CA
|
|
#7
|
Stanford Health Care-Stanford Hospital
|
Stanford, CA
|
|
#8
|
Houston Methodist Hospital
|
Houston, TX
|
|
#9
|
Hospitals of the University of Pennsylvania-Penn Presbyterian
|
Philadelphia, PA
|
|
#10
|
Beaumont Hospital-Royal Oak
|
Royal Oak, MI
|
Hospital Ranking information as of May 12th, 2017